Posted
Photo:
Opioids are used in painkillers such as codeine, oxycontin and fentanyl, among others. (AP: Jessica Hill)
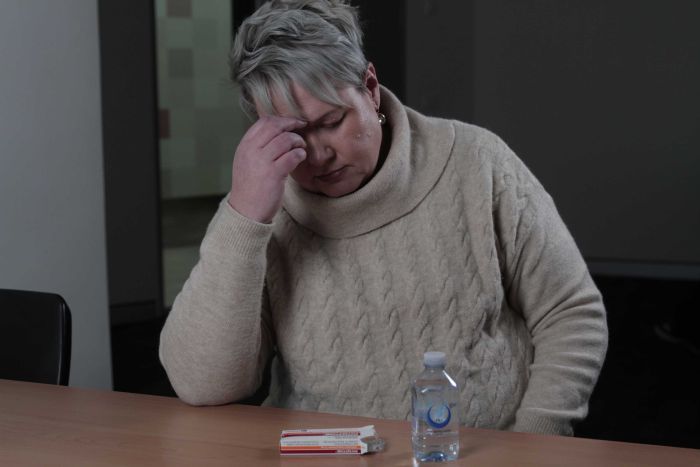
Patients using painkillers and doctors prescribing them have been put on notice by the Federal Government, as it tries to head off a US-style opioid epidemic.
Key points:
- A government crackdown on prescription opioids is leaving some chronic pain sufferers without access to painkillers
- Patients say some doctors are avoiding prescribing opioid-based painkillers
- Nearly 5,000 GPs received a warning that their prescribing of opioids was being monitored
But the crackdown is leaving some sufferers of chronic pain without access to painkillers.
Jodie Carter hasn’t been able to get a prescription to deal with her chronic pain since March, when her doctor received a government letter telling him to cut down her opioid pain medication.
“I don’t know what the future holds, I don’t know how I am going to function, I don’t know how I am going to finish uni,” Jodie Carter told 7.30.
“I don’t know how I’m going to look after my kids.”
She has been stretching her last prescription out but now only has a week’s worth of pills left.
‘Nothing else has worked for me’
Ms Carter has debilitating nerve pain in one arm and intercostal neuralgia.
She has been prescribed opioids to control the pain for 25 years.
“I’ve tried other things,” she said.
“I’ve tried interventions that are outside the scope of opiates, but nothing other than that has worked for me.”
Since her doctor told her he would no longer see her as a patient, following the letter he received she has tried other GPs, but no-one will write her a script.
Now she has been told she will need to go to a methadone clinic.
“It only takes one person to see me who can make assumptions,” she said.
“It’s just made my own self-esteem drop to think that I’ve had to reach those levels just to get medication.”
A thousand avoidable deaths
Photo:
Chief Medical Officer Brendan Murphy had written to doctors warning them about overprescribing opioids. (ABC News)
In July last year the Australian Government’s Chief Medical Officer, Brendan Murphy, sent letters to almost 5,000 GPs warning them their prescriptions of opioids were being monitored.
Last week the government announced it would be making post-operative opioid pack sizes smaller, and is changing indications for the powerful narcotic fentanyl so it can only be used for cancer and palliative care patients.
“We do not want Australia to be in the situation of America,” Professor Murphy told 7.30.
Opioids in Australia
- In 2016, 1,045 Australians died from opioid overdose
- Of those, 712 were attributed to pharmaceutical opioids like morphine, codeine, oxycodone, fentanyl and tramadol
- The overdose rate rose from 3.8 to 6.6 per 1,000,000 people between 2007 and 2016
- The highest death rates were between ages 35 and 44 and among males
*NDARC and AIHW
“We have a thousand opioid related overdose deaths a year in Australia, that is a thousand avoidable deaths.”
In the United States more than 900 people die each week from opioid overdoses.
Despite outcry from GPs, Professor Murphy defended his letter.
“All we were saying was, these are the data, look at your practise and reflect,” he said.
“And if you’re using opioids in non-cancer chronic pain, you should consider your practise and modify your practise.”
But for some doctors it felt like more than just gentle advice to review their prescribing.
“It felt quite threatening,” Kate Shapland told 7.30.
“It didn’t come across as, could you examine your practise.”
‘More risk for patients to suddenly stop’
Photo:
Dr Kate Shapland has taken on dozens of new patients who have been dumped by their normal GP. (ABC News)
Dr Shapland said the letter took no account of the doctor-patient relationship.
“I felt that it was a letter from someone unknown… they didn’t know my patients, they didn’t know how much it affected their life, they didn’t know how much I was trying to reduce their medication or how much concern I put in, so I just thought a letter out of the blue from a statistic was quite rude.”
Dr Shapland has taken on almost 30 new patients with chronic pain who had been dumped by their usual GP after the crackdown.
“Unfortunately what happened was some of my colleagues did decide that they weren’t going to see people anymore,” she said.
“So a few people came and approached me and asked would I be prepared to take them on.
“I feel I might be at risk, an audit from Medicare seems to be bandied about a lot, however I just felt clinically it would be more risk for patients to suddenly stop.”
Dr Paresh Gwada is another who received the warning letter.
The Canberra GP specialises in aged and palliative care, and says he would rather risk an audit than see people die in pain.
He has also taken on more patients who dropped by their own doctors.
“It’s really a shift of the problem,” he told 7.30.
“It doesn’t necessarily mean that the total number of opioid prescribing has gone down or that that patient is having appropriate treatment, appropriate medication.”
In second letter published this June, Professor Murphy apologised for upsetting GPs with his first written warning but defended its intent.
“I would imagine that a mature and sensible GP who is practising in aged or palliative care would read the correspondence that we sent them in an entirely appropriate way, and keep doing what they’re doing,” he said.
“We didn’t want to upset them.”
Topics:
health,
drug-use,
addictive,
pharmaceuticals,
pain,
australia